Bacillus anthracis, the causative agent for anthrax, is a Category A pathogen and its ability to be used as a bio-terror agent was confirmed by the October 2001 postal attacks in the United States in which finely ground anthrax was mailed to political offices and news stations at the East coast. This resulted in 18 confirmed cases of anthrax (11 inhalation, 7 cutaneous), caused US Congress to be shut-down for several days and led to general public panic about possible other anthrax attacks. Fortunately, this was a small event. However, in assessing the threat and damage from a large scale anthrax attack, a 1993 US Congressional Office of Technology report estimated that the release of 100 kg of anthrax spores up wind of Washington D.C. would result in 130,000-3,000,000 deaths. Furthermore, using an economic model from the CDC, it was estimated that the cost of such an attack would be $26.2 Billion/100,000 people. It leaves little doubt that release of anthrax onto any developed population would lead to similar primary and secondary problems.
Human anthrax has three major clinical forms depending on the route of infection, cutaneous anthrax, gastrointestinal anthrax and inhalation or respiratory anthrax. If untreated, all forms of anthrax can lead to septicemia, hemorrhagic meningitis, and death. Inhalation anthrax is by far the most dangerous form; case-fatality rates are high, even with appropriate antibiotics and supportive care. Among cases of non-intentional inhalation anthrax during the twentieth century, the overall case fatality was >75%. Following the bioterrorist attack in October 2001, the case-fatality rate among patients with inhalation disease was 45% (5/11) due to an awareness after the first case and an early and vigorous antibiotics treatment regimen.
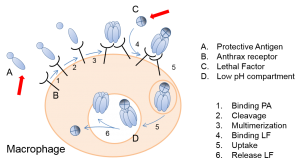
Bacillus anthracis is an aerobic, rod-shaped, encapsulated, spore-forming bacterium. The most deadly form of the disease is contracted through the inhalation of the spores. Once the spores have entered the lung, they are ingested by macrophages. Some of the spores are destroyed, but a number survive and are transported via lymphatics to lymph nodes draining the lungs. On their journey and upon arrival, the spores germinate, kill their host cells, multiply and produce toxin. Disease subsequently becomes manifest after about 10 days with death ensuing between days 12 and 14. Based on primate data, it has been estimated that for humans the LD50 is 2,500 to 55,000 inhaled anthrax spores. Replicating bacteria release toxins leading to hemorrhage, edema and necrosis. The lethal toxin produced by B. anthracis consists of a target cell binding component called Protective Antigen (PA), and a deadly component called Lethal Factor (LF). This lethal toxin is Bacillus anthracis’ major killing factor. In exposed animals, it has been shown that once toxin production has reached a critical threshold, death occurs even if bloodstream sterility is achieved with antibiotics. For this reason, an NIH panel of experts on anthrax has issued that neutralization of the anthrax toxin is an absolute requirement for the successful treatment of anthrax and that human immunoglobulins or monoclonal antibodies are ideal candidates for this purpose. Since then, there has been a focus on the generation and development of anthrax antitoxins. The NIH panel also recommended that preferably these antitoxins should be directed against different toxin epitopes or components. Most of the antitoxin focus, however, has been on the development of single antitoxins.